What is Strabismus?
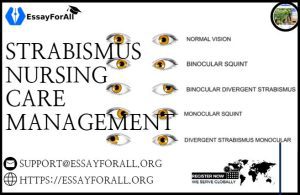
Strabismus is a vision disorder associated with misalignment of the eyes to the point that they point in different directions. In this case, an inward deviation of eyes can make it difficult for an individual to align their eyes for binocular vision leading to double vision. Strabismus is associated with the abnormal development of eye movements, motion processing, and stereopsis. However, the exact cause of the condition is not known yet, making it challenging to develop an effective treatment strategy.
Pathophysiology of Strabismus
Although the exact cause of strabismus is not yet known:
- Esotropia is believed to be an inborn and irreversible fusion defect.
- It is dysfunction and maldevelopment of binocular sensitivity.
- Chavasse countered this assertion and argued that the neural components responsible for binocular vision are present at birth, but abnormalities in optical input affect the development of fusion.
- Other authors argue that neural factors as the cause of strabismus, where the brain has a problem controlling eye movement due to imbalances and weakness of muscles and nerve pathways that control eye movement.
- Researchers also assert refractive errors as causes of strabismus, where farsightedness, astigmatism, and nearsightedness contribute to the condition by making it difficult for eyes to maintain proper alignment.
- Neurological disorders, including conditions such as strokes, brain tumors, cerebral palsy, and others, could also lead to strabismus development by affecting the brain’s normal functioning and the nervous system.
- Although there are many causes and mechanisms behind the development of strabismus, and their understanding has come a long way, there is still more to learn to understand the condition clearly.
Strabismus Statistics
The prevalence of strabismus in the US and the world is as shown:
- Data shows that strabismus is the most prevalent ocular condition among young children. For instance, the condition affects five people in every 100 citizens in the US. This means about 12 million out of the 245 million people in the US have strabismus.
- Although strabismus distribution is equal among genders (males and females), the condition is more prevalent among whites than African Americans
- Another study conducted between 1965 and 1994 indicated that strabismus prevalence was 1 in 403 or 25 in every 10,000 live births.
- To establish whether infants are born with esotropia or it develops later, Nixon et al. observed over 1200 alert infants in a newborn nursery at a hospital. The findings were that about 3.2% of the babies (40) had esotropia, including intermittent esotropia, variable esotropia, and varying esotropia and exotropia.
- The conclusion is that strabismus can be observed/identified in infants before they reach six months.
Causes of Strabismus
Although the actual cause of strabismus is not yet known, the condition is believed to be caused by the following:
- Genetics: Having a family member with strabismus increases the risk of developing the condition.
- Loci susceptibility: Researchers suggest a relationship between non-syndromic strabismus and loci susceptibility, mainly in regions 3p26.3 to 26.2 and 6q24.3 to 25.1.
- Uncorrected refractive errors: Refractive errors such as farsightedness, astigmatism, and nearsightedness cause strabismus making it difficult for eyes to maintain proper alignment.
- Neurological: Problems due to nervous system issues and damage to the brain area responsible for controlling eye movement
- Neurological Conditions: Conditions including stroke, Down’s syndrome, cerebral palsy, and brain tumors are other major causes of
Clinical Manifestations of Strabismus
Strabismus manifests with a range of ocular motor signs, including:
- This is a condition where one or both eyes point inwards hence they don’t line up correctly.
- Pursuit asymmetry
- Latent nystagmus: This is common in people with congenital esotropia.
- This refers to reduced vision in one eye due to abnormal vision development during childhood.
- Uncoordinated eye movement
- Double vision
Nursing Assessment and Diagnostic Findings
The following tests and procedures can be used to diagnose strabismus and determine the extent of the problem:
- The light reflex test: This test involves sitting the child on their parent’s lap and using a small light about one meter in front of the child. Once the child’s attention is directed to the light, the doctor notes and compares the light reflection in each eye. Identical light reflection in each eye indicates normal eye alignment, while deflection of the light reflex indicates abnormal ocular alignment.
- The red reflex test: In this test, the doctor uses a direct ophthalmoscope and uses it to direct attention to the child. The doctor then observes the red reflexes on both eyes to establish whether they are identical in terms of size, shape, and color.
- Alternate prism cover test: In this test, the doctor holds an object in front of the child capturing the child`s attention. The doctor then covers one eye to establish whether the uncovered eye makes a corrective movement. Strabismus is deemed present when the eye makes a corrective movement. This test is used to help measure the exact angle of the strabismus. The procedure can help establish the full magnitude of esotropia and esophoria.
- The Uncover test: In this test, the doctor covers one eye and uses an object, such as a toy, to draw the child’s attention. The eye covering is then removed, and the eye is visualized for any adjustments. If the eye returns make adjustments to return to correct fixation, the eye is deemed to be misaligned.
Medical Management of Strabismus
The medical management of strabismus includes the following:
- Prism Lenses. Small deviations in ocular alignment may be corrected with prism lenses. Occlusion therapy could be considered in the case of amblyopia.
- Corrective lenses. This lens is worn to improve daily vision and helps correct refractive errors such as hyperopia, myopia, presbyopia, and astigmatism.
- Occlusion therapy. This approach is used to enhance the vision of the lazy eye in children. It involves covering or patching the normally aligned eye for a few hours daily to help the other eye correct itself.
- This is a medication used for paralyzing the ciliary muscles to relax accommodation. This helps relax the eye allowing alignment. The drug is a combination of cyclopentolate (1%) and phenylephrine (2.5%).
- Botulinum toxin (BOTOX) Injection. In some cases, BOTOX injection may be used to stop muscles around the eye from working for some time to improve eye alignment and promote better vision. It is used as an alternative to surgery.
Nursing Management of Strabismus
The nursing care management of a child with strabismus includes:
Nursing Assessment
The assessment of strabismus includes:
- Assessing the child’s history. Various risk factors are associated with strabismus, among them, being:
- Prematurity
- History of systemic disorders and use of systemic medications
- Perinatal or gestational complications
- History of secondary ocular
- Family history of strabismus
- Male sex
- Physical examination. The nurse examines the child for various clinical presentations, including central scotomas, incomitance, amblyopia, and impaired binocularity.
Nursing Diagnoses of Strabismus
The nursing diagnoses for strabismus include:
- Disturbed visual perception related to abnormal ocular alignment.
- Injury risk related due to impaired vision.
- Social isolation is related to the individual’s inability to participate in social activities due to impaired vision.
- Knowledge deficit relating to impaired vision.
Nursing Care Planning and Goals for Patients with Strabismus
The nursing care planning and goals for patients with strabismus include the following:
- The patient will restore their sensory perception function.
- The patient will be free from any form of injury related to impaired vision.
- The patient will be able to interact freely with others and engage in social activities.
- The patient will better understand strabismus and its treatment approaches.
Nursing Interventions for Strabismus Patients
- Patch therapy. This is a form of treatment that involves covering the stronger eye to encourage the use of the weaker eye. This treatment is effective since it helps children strengthen the sight and alignment of the weaker eye. The earlier the treatment starts, the faster and stronger the eye gets.
- Vision therapy. This is a treatment that targets at improving the visual abilities of the eyes. It involves exercises performed with the doctor’s supervision to help improve how the eyes process visual information rather than strengthening the eye muscles.
- Injury Prevention. The nurse ensures the patient conforms to the surrounding. The nurse also puts a call light within the patient’s reach and instructs the patient on how to call for help. The nurse should respond to the call light immediately. Educating the patient about home safety, including using proper lighting at home, handrails, and other safety measures.
- Enforce the patient and caregiver knowledge.
- The nurse should observe and note existing misconceptions about strabismus.
- Understanding and acknowledging racial/ethnic differences is crucial during care.
- Consider the patient’s/caregiver’s readiness to learn and learning style
- Include the patient/caregiver in the treatment plan by establishing the learning goals and objectives together.
- Provide clear and understandable instructions, explanations, and demonstrations.
Nursing Evaluation for Strabismus
The nursing evaluation to establish whether nursing care goals were met includes:
- The patient will have restored sensory perception functioning.
- The patient will be free from injury throughout the treatment period.
- The patient will be interacting socially with others.
- The patient will have a better understanding of strabismus, including the treatment and surgery options.
Nursing Documentation Guideline
- Provide baseline and subsequent assessment, including the signs and symptoms.
- Document the patient’s religious and cultural restrictions to care and personal preferences.
- Document the plan of care and the people involved in developing and implementing it.
- Document the patient’s/caregiver’s teaching plan.
- Document the patient’s response to interventions.
- Document the patient’s progress
- Indicate the long-term needs of the patient and those responsible for taking action.
Also Read: Pancreatitis Nursing Care and Management