Sepsis Essays
Sepsis Essays homework help is something many nursing students look for when they start covering infections, deterioration, and critical care. The topic can feel heavy. Sometimes even frightening, because sepsis is not theoretical.
We see it in real wards. We hear stories from senior nurses who watched patients change within hours. So, when assignments start asking you to explain causes, early signs, and treatment decisions, the work can feel personal. We understand that feeling. Our role here is to help you learn the subject in a way that feels practical rather than overwhelming.
We have spoken with many students who say the same thing: “I know what sepsis is, but I don’t feel confident writing about it in detail.” That is usually because the condition progresses quickly and affects different people in different ways.
There are assignments that ask you to compare cases, or reflect on deterioration, or outline escalation. Some students try to memorise lists of signs and symptoms but still feel unsure. We try to support students by helping them break the topic into small, clear points that reflect real clinical thinking rather than just notes from a textbook.
Understanding Sepsis in Simple Terms
Sepsis is the body reacting in a harmful way to an infection. Instead of controlling the infection, the immune response becomes too strong and starts to damage tissues and organs. Many people first hear about sepsis in emergency or critical care units, but it can start anywhere. A small wound. A chest infection. A urinary tract problem. A surgical site that seemed fine at first.
One thing that makes sepsis challenging is that early signs can look like flu or a cold. People sometimes explain this away, thinking they just feel a bit unwell. By the time the signs feel severe, the body may already be struggling.
This is why nursing students are taught:
- Know the early signs
- Speak up early
- Do not wait to “see what happens”
It feels simple. But in real practice, it can be hard to tell. Especially when patients cannot describe how they feel, such as infants, older adults, or those with communication difficulties.
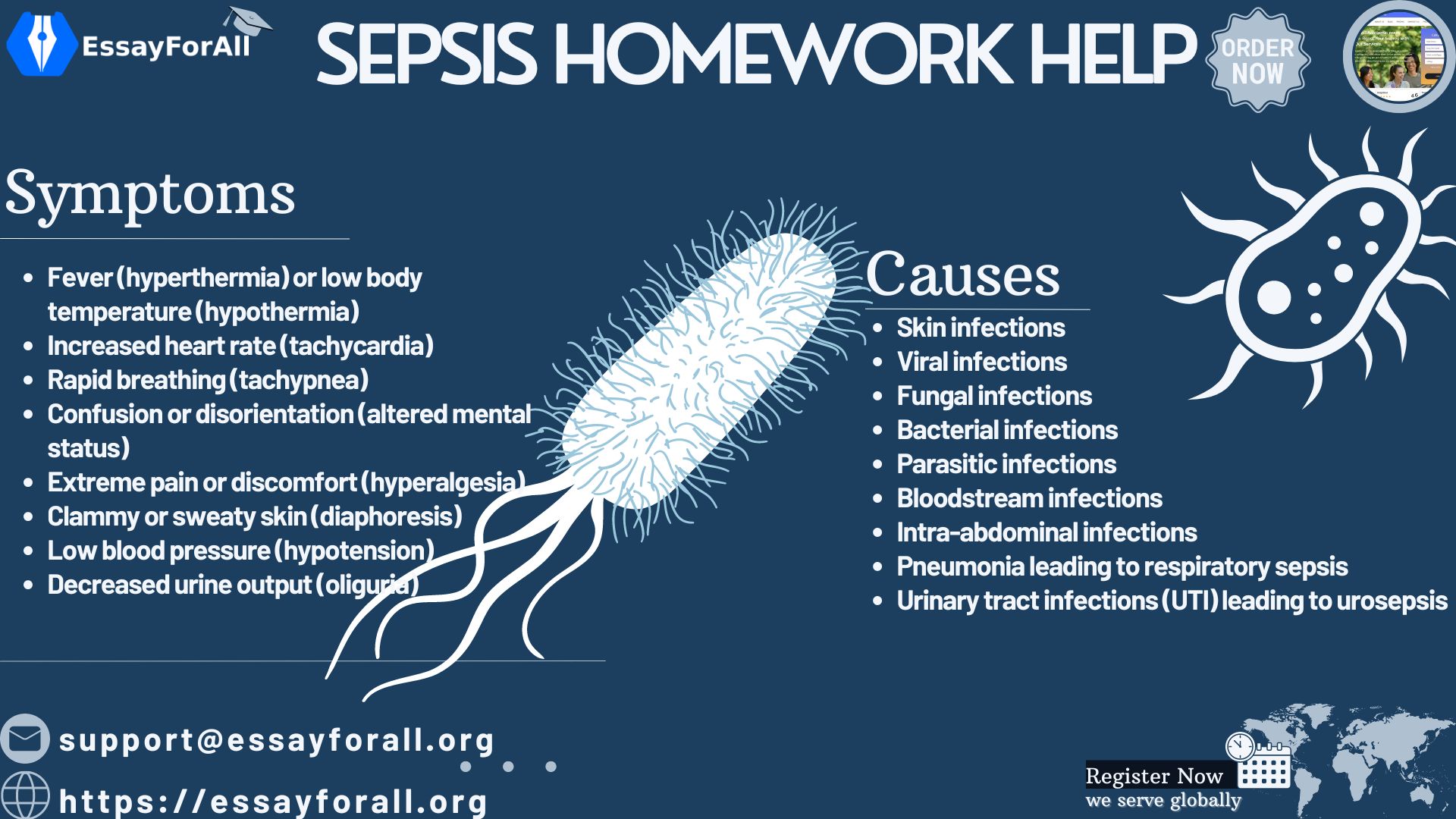
Symptoms: Recognising Possible Sepsis
Different groups show signs in different ways. One symptom list for everyone can sometimes cause confusion. The table below might help separate how symptoms show in different age groups.
Symptoms of Possible Sepsis by Age Group
| Group | Signs to Look For | Notes |
|---|---|---|
| Adults & older children | Breathing faster, confusion, fever, chills, blotchy or pale skin, fast heartbeat | Confusion is often an overlooked early sign in adults |
| Babies & toddlers | Hard to wake, weak or very high-pitched cry, difficulty feeding, cold hands and feet | Parents often say “they seem different” even if the signs seem small |
| Older adults | Sudden confusion, reduced speech clarity, extreme tiredness, change in toilet habits | Symptoms may look like dementia or fatigue, making early recognition harder |
We sometimes think of sepsis as dramatic and obvious. But many nurses describe the first signs as quiet. A patient just seems “off.” You might find yourself staring at their face for a bit longer than usual, trying to work out what changed. This is where nursing judgement grows: not from memorising lists, but from noticing small changes.
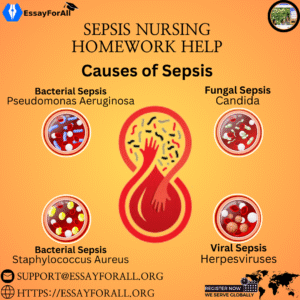
What Can Cause Sepsis
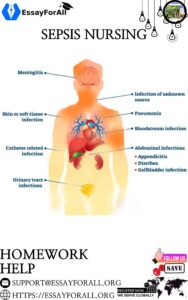
Most cases start with infections. Bacterial infections are the most common source, though viruses, fungi, and parasites can lead to the same outcome. The infection can start almost anywhere:
- Skin: even small cuts can allow bacteria in. Catheters, dressings, and open wounds are common entry points.
- Urinary tract: dehydration, catheter use, and kidney issues increase the chance.
- Lungs: pneumonia is one of the well-known causes.
- Abdominal organs: gall bladder infections, bowel issues, appendix problems.
Something students sometimes forget is that how long the infection has been present matters as much as what type of infection it is. A small infection ignored for too long has more chance of leading to sepsis than a larger infection treated early.
And sometimes, people delay seeking care because they think they’ll get better on their own. We all know someone who says, “I’ll be fine in a few days.” That mindset can be risky with sepsis.
The Stages of Sepsis
Sepsis does not happen all at once. It usually follows a progression. The clearer you understand this sequence, the easier it becomes to explain in essays or exams.
Stages of Sepsis and What Happens
| Stage | What You May See | What Is Happening in the Body | Typical Clinical Actions |
|---|---|---|---|
| Sepsis | Fever, fast breathing, fast heart rate, confirmed infection | The immune system is reacting strongly | Start antibiotics and fluids, close monitoring |
| Severe Sepsis | Signs of organ stress: low urine output, irregular heartbeat, cold or patchy skin, extreme weakness | The reaction is affecting organ function | Increased monitoring, oxygen, targeted treatment |
| Septic Shock | Very low blood pressure, confusion, risk of organ failure | The body can no longer maintain blood pressure or supply oxygen effectively | Intensive care treatment, vasopressor medication, high level monitoring |
Many nursing students say the hardest part is identifying the shift from sepsis to severe sepsis. The change can be gradual or fast. In clinical care, nurses look for:
- Urine output dropping
- Mental state changing
- Skin colour or temperature changes
These signs are sometimes more telling than a thermometer or blood pressure reading.
Who Is Most at Risk?
Some people are more likely to develop sepsis:
- Babies and older adults
- People with long-term health conditions like diabetes or cancer
- People with weak immune systems
- People recovering from surgery or long hospital stays
- People living with malnutrition
- People with large wounds or burns
Something we sometimes forget is how much social conditions matter. People without easy access to healthcare are more likely to delay treatment. This delay can change everything. It’s not always biology; sometimes it’s circumstance.
You may have seen this during placements. A patient arrives later than they should because they could not travel sooner or hoped to avoid hospital. This doesn’t mean the patient made a mistake. It means care must adapt to real human situations.
Diagnosing Sepsis
Doctors and nurses use a combination of:
- Patient history
- Physical signs
- Blood tests
- Urine tests
- Imaging such as x-ray, MRI, or CT
Some blood tests check for infection. Some look at how organs are coping. A high lactate level, for example, suggests the tissues are not getting enough oxygen. These results help staff decide how urgent the situation is.
The tricky part is timing. Early treatment can change the entire outcome. Waiting to “see what happens” is rarely safe.
Treatment
People with sepsis usually need:
- Fluids to support blood pressure
- Antibiotics
- Pain relief
- Possible oxygen therapy
- Sometimes vasopressor medication to support the circulation
Nurses play a central role during treatment. They notice small changes. They watch how the patient responds. They record urine output, behaviour changes, breathing patterns. These details often guide the next step more than any single lab result.
Recovery and Life After Sepsis
Recovery is not the same for everyone. Some people feel better quickly. Others describe feeling tired for months. A few individuals experience memory problems, sleep disruption, or mood shifts. This is sometimes referred to as post-sepsis effects or post-sepsis syndrome.
It can leave a person feeling different from before the illness. Families notice these changes too. The emotional side is real, and sometimes it is the part nursing students remember most when they reflect on patient stories.
100 strong, research-ready Sepsis capstone project topics
A. Clinical Management & Diagnosis
- Early Recognition of Sepsis in Emergency Departments
- Challenges in Diagnosing Sepsis in Resource-Limited Hospitals
- Role of Rapid Lactate Testing in Early Sepsis Detection
- Use of Sequential Organ Failure Assessment (SOFA) Score in Sepsis Diagnosis
- Comparison of qSOFA vs SIRS Criteria in Identifying Sepsis Risk
- Point-of-Care Testing for Sepsis Biomarkers
- Diagnostic Delays and Their Impact on Sepsis Mortality
- Role of Artificial Intelligence in Predicting Sepsis Onset
- Early Warning Score Systems for Sepsis Detection in ICU
- Antibiotic Stewardship and Its Impact on Sepsis Outcomes
- Evaluating Triage Protocols for Sepsis in Accident & Emergency Units
- Effectiveness of Rapid Response Teams in Reducing Sepsis Complications
- Bedside Ultrasound Use in Sepsis Assessment
- Clinical Decision Support Tools for Sepsis Identification
- Identifying Sepsis in Patients with Multiple Comorbidities
B. Treatment & Therapeutic Strategies
- Effectiveness of Fluid Resuscitation Protocols in Sepsis Treatment
- Analysis of Vasopressor Use in Septic Shock
- Corticosteroid Use in Severe Sepsis: Benefits vs Risks
- Timing of Antibiotic Administration and Patient Survival Rates
- Personalized Medicine Approaches to Sepsis Care
- Comparing Crystalloids vs Colloids in Sepsis Resuscitation
- Nutrition Support Therapy for Sepsis Patients in ICU
- Hemodynamic Monitoring Techniques in Sepsis Care
- Blood Purification Therapy in Septic Shock
- Role of Immunotherapy in Sepsis Treatment
- Sedation Strategies and Outcomes in Septic Patients on Ventilators
- Extracorporeal Membrane Oxygenation (ECMO) in Severe Sepsis
- Managing Sepsis in Patients with Renal Failure
- Use of Probiotics in Reducing Sepsis Incidence in ICU
- Role of Physiotherapy in Sepsis Recovery
- Sepsis Bundles Implementation and Outcome Evaluation
- Post-ICU Rehabilitation in Sepsis Survivors
C. Microbiology & Pathophysiology
- Host–Pathogen Interactions in Sepsis Development
- Role of Endotoxins in Septic Shock Progression
- Immune System Dysregulation in Sepsis
- Antimicrobial Resistance and Sepsis Mortality
- Biofilm Formation and Its Role in Sepsis Infections
- Emerging Multidrug-Resistant Bacteria in Sepsis Cases
- Sepsis Caused by Fungal Infections: Challenges in Diagnosis
- Role of Viral Pathogens in Sepsis (Focus on COVID-19 Link)
- Differences Between Gram-Positive and Gram-Negative Sepsis
- Genetic Predisposition to Severe Sepsis
- Cytokine Storm Mechanisms in Septic Shock
- Relationship Between Sepsis and Multi-Organ Failure
- Molecular Biomarkers Under Development for Sepsis Detection
- Microbial Profiling in Neonatal Sepsis
- Pathophysiology of Sepsis-Induced Cardiomyopathy
- Role of Gut Microbiome in Sepsis Susceptibility
D. Sepsis in Special Populations
- Neonatal Sepsis: Early Indicators and Management
- Sepsis in Children Under 5 Years: Risk Factors and Outcomes
- Sepsis in Pregnant Women and Postpartum Patients
- Sepsis in Elderly Patients with Chronic Illness
- Sepsis and HIV Co-Infection Outcomes
- Sepsis in Cancer Patients Undergoing Chemotherapy
- Challenges in Managing Sepsis in Diabetic Patients
- Sepsis among ICU Surgical Patients
- Gender-Based Differences in Sepsis Outcomes
- Sepsis in Patients with Autoimmune Diseases
- Sepsis in Intensive Care Trauma Patients
- Sepsis in Burn Injury Patients
- Healthcare-Associated Sepsis in Long-Term Care Facilities
- Sepsis in Malnourished Populations
- Impact of Obesity on Sepsis Recovery
- Sepsis in Individuals with Drug or Alcohol Dependence
- Sepsis in Organ Transplant Recipients
- Sepsis Outcomes in Rural vs Urban Healthcare Settings
E. Prevention & Public Health
- Hand Hygiene Compliance and Sepsis Prevention
- Importance of Infection Control Protocols in Healthcare
- Vaccination Campaigns and Their Role in Reducing Sepsis Rates
- Safe Delivery Practices to Prevent Neonatal Sepsis
- Preventing Sepsis Through Early Infection Treatment
- Impact of Public Awareness Campaigns on Sepsis Recognition
- Community Education Strategies for Sepsis Prevention
- Hospital Environmental Sanitation and Sepsis Reduction
- Screening High-Risk Patients for Sepsis
- Role of Clean Water Access and Sepsis Risk in Low-Income Areas
- Antibiotic Misuse and Rising Sepsis Burden
- Prevention of Sepsis in Surgical Wards
- Reducing Ventilator-Associated Sepsis in ICU
- Impact of Healthcare Worker Training on Sepsis Outcomes
- Early Discharge Follow-Up to Prevent Sepsis Readmission
- Digital Apps for Public Sepsis Awareness
- Economic Impact of Sepsis on Healthcare Systems
- Integrating Sepsis Prevention into National Healthcare Policies
F. Nursing Care, Psychological Impact & Patient Experience
- Nursing Assessment Tools for Early Sepsis Detection
- Nurse-Led Sepsis Screening Programs in Wards
- Nurse Training and Clinical Competency in Sepsis Care
- Patient and Family Education on Sepsis Warning Signs
- Psychological Effects of Sepsis on Survivors
- Caregiver Stress in Managing Sepsis Patients
- Communication Challenges in Sepsis Emergency Care
- Ethical Challenges in Treating Terminal Sepsis Cases
- Telemedicine Use in Remote Sepsis Monitoring
- Experiences of Sepsis Survivors During Rehabilitation
- Patient-Centered Care Approaches in Sepsis Management
- Burnout Among Nurses Caring for Sepsis Patients
- Holistic Care Approaches for Sepsis Recovery
- Case Study Review: Sepsis-Related Medical Negligence Claims
- Role of Interprofessional Collaboration in Sepsis Management
- Patient Narratives and Storytelling in Understanding Sepsis Trauma
Why Students Ask for Help With Sepsis Essays
Sepsis assignments ask you to combine:
- Biological understanding
- Clinical signs
- Nursing priorities
- Human experience
That is a lot to hold at once. Some students feel pressured to write perfectly, and that pressure makes thinking harder. We help by guiding your structure, suggesting what to include, and helping you express your understanding clearly. You are not just writing to pass. You are learning to think like a nurse who recognises early deterioration and speaks up.